plantar fasciititis
What is plantar fasciitis?
Plantar fasciitis is a common and often painful foot condition that affects millions of people worldwide. The vast majority of people who experience plantar fasciitis are active adults between the ages of 25 and 65 years old.
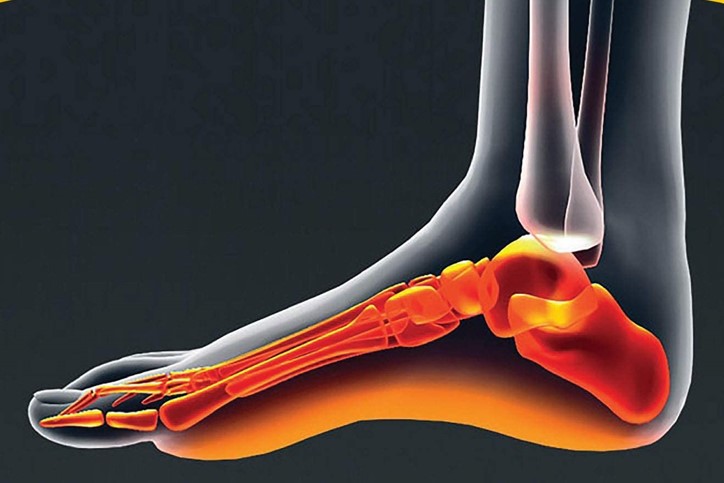
Plantar fasciitis occurs when the plantar fascia, a fibrous band of tissue on the bottom of the foot that helps to support the arch, is overloaded or overstretched. With overuse or over time, the fascia loses some of its elasticity or resilience and can become inflamed, resulting in pain.
What are the symptoms of plantar fasciitis?
Plantar fasciitis symptoms can develop gradually over time or, in some cases, develop suddenly after engaging in intense physical activity. Recognizing symptoms is essential for early intervention and proper management.
It's important to keep in mind that the severity and duration of symptoms can vary from person to person. The most common symptoms of plantar fasciitis include:
- Pain on the bottom of the foot, near the heel. This is the most prevalent and telltale sign of plantar fasciitis. This pain can be a dull ache or a sharp, stabbing sensation. The arch along the bottom of the foot may also ache or burn.
- Severe heel or foot discomfort after getting out of bed in the morning, or after extended periods of rest. This pain tends to subside after a few minutes of walking.
- Heel or foot pain that tends to worsen after physical activity but is not typically experienced during exercise. Climbing stairs can be particularly painful.
- Tenderness when touching the affected area, especially near the heel.
- Stiffness in the foot is common, particularly upon waking up or after prolonged periods of sitting. This stiffness can make it difficult to walk comfortably.
What causes plantar fasciitis?
Plantar fasciitis occurs when the thick band of tissue on the bottom of your foot (the fascia) becomes overstretched or experiences excessive strain caused by repetitive stress from activities like standing or running. It can also occur if there is a significant weight gain, including during pregnancy.
This constant stretching and strain of the plantar fascia can lead to chronic degeneration, or the development of small tears in the fascia fibers, particularly where the fascia connects to the heel bone. In addition to tears, ultrasound evaluations often show calcifications, and thickening of the plantar fascia.
Certain risk factors can make you more susceptible to plantar fasciitis:
- foot arch problems (both flat feet and high arches)
- long-distance or downhill running on uneven surfaces
- excess weight
- a tight Achilles tendon
- shoes with inadequate arch support or soft soles
- abrupt changes in activity levels.
Plantar fasciitis diagnosis
If you suspect you have plantar fasciitis or are experiencing persistent foot pain, you should see your doctor for a proper diagnosis and treatment plan. Early intervention and appropriate management can help alleviate symptoms and improve your quality of life.
Your doctor will examine your foot, looking for the following signs or risk factors of plantar fasciitis:
- an area of maximum tenderness on the bottom of your foot, just in front of your heel bone
- a high arch or flat foot (a risk factor)
- limited dorsiflexion, or "up" motion, in your ankle
- the absence of symptoms from other foot conditions that may share similar symptoms with plantar fasciitis, such as insertional Achilles tendinitis, calcaneal (heel) stress fracture, or plantar nerve entrapment.
In addition to a physical exam of your foot, your doctor may consider obtaining x-rays or ultrasound evaluation if your history or physical exam indicates other injuries or conditions such as heel spurs, fractures, or arthritis. Additionally, ultrasound may show thickening and swelling of the plantar fascia, which is a typical feature of the condition.
Your doctor may also consider ordering magnetic resonance imaging (MRI) or ultrasound if your pain is not relieved by initial treatment methods, or if your doctor is concerned that a different problem is causing your pain.